If you read only one online ACA guide this year, make sure it’s this one!
There are lots of ‘essential’ ACA guides out there. Many are confusing. Some contain errors. As if ACA governance, risk management & compliance weren’t complicated enough. Getting things wrong can prove very costly. So we’ve done our best to stick here to key IRS changes, important tips & some common errors as employers turn the final bend of TY23 ACA Compliance.
If you do have questions about topics not covered here — such as past penalties, specific HCM data flows, filings for an aggregated ALE — please do not hesitate to contact BENEFITSCAPE, the leading specialist in ACA compliance thanks to proven regtech and unrivalled ACA experience.
BENEFITSCAPE’s experts are always happy to help.
NO MORE PAPER FILING
For TY23, the maximum number of paper returns to the IRS per Applicable Large Employers [ALE] is 10, down from 250. So all ALEs will now need to e-file their FORM 1094 and all FORMs 1095 via the IRS ACA Information Returns [IRSAIR] system.
» TIP: Only IRS-certified e-filers can file to the IRSAIR. It is important to confirm your ACA vendor has a certified Transmission Control Code [TCC].
TECH, PROCESS, RISK
No HCM, even with an ACA module, does all the ACA work for you. Of course not. Tech is a tool. Even the magic worked on HCMs by BENEFITSCAPE ACA_regtech* needs oversight by BENEFITSCAPE experts.
You must be confident your ACA vendor has the proven experience of ACA governance, risk management, and compliance to take on board the latest IRS regs & requirements as well as your company’s unique business rules, health plan provisions, and employee population.
» TIP: Do not green IRS filing unless you are 100% confident any gaps, anomalies, or other data processing issues have been addressed. That’s why ACA_regtech* runs Flag & Fix diagnostics throughout the ACA process and a full pre-submission simulation of all IRS filings.
COMMON ERRORS: FORM 1094-C
All ALEs must submit an employer FORM 1094-C to the IRS providing basic information about the ALE and its health coverage for employees.
Employees don’t get sent this form.
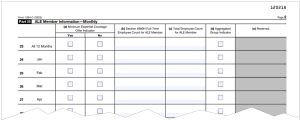
Most FORM 1094-C errors occur in Part III, Column [a], capturing whether the ALE offered medical coverage to at least 95 percent of its full-time employees in each month of the calendar year.
» TIP: Part III, Column [a] should be carefully reviewed before submission to the IRS. Here are some common errors made by reporting vendors: Despite indicating YES in the initial ‘All 12 Months’ check box, the subsequent month-by-month boxes are left blank or some ticked NO. If ‘All 12 Months’ is ticked YES, then all the month-by-month boxes need to be ticked YES too. [See image below.]
COMMON ERRORS: FORMs 1095-C
FORMs 1095-C are specific to each individual employee of an ALE with full-time status for at least one month of the reporting tax year.
Part II of FORM 1095-C identifies for each month whether an Offer of Coverage was made to the employee, the employee’s own contribution amount [for self-only coverage], and an IRS Code denoting this offer and coverage status of the employee.
FORMs 1095-C are completed and sent to employees by the ALE, who then also submits them to the IRS along with the transmittal form. If an employee has full-time status for at least one month, all months must be coded on the form.
Some common FORM 1095-C pitfalls and questions are addressed below. If you have other questions, please feel free to contact BENEFITSCAPE.
- LINE 16 must never be left blank if an applicable IRS Code is available. If Offer of Coverage qualifies as affordable but is waived by the employee, the employer should still enter an Affordability Code. If Code 1A (Qualifying Offer) is entered in LINE 14, then enter Code 2G (Federal Poverty Line Safe Harbor) in LINE 16 (even if the instructions seem to indicate a Code is not necessary].
- Short-term employees working 30 or more hours per week are considered full-time employees under the ACA, even if they only work 3 or 4 months and however classified (for example, short-term, temporary, interns, or co-op employees). They are NOT considered variable hour employees.
- Variable Hour (VH) employee’ is an ACA term referring to a new hire who, at the time of hire, the employer cannot reasonably determine whether the employee will work full-time hours. The VH designation is usually used with the Look Back method [see below] for determining full-time status.
- Self-employed individuals are not considered W-2 employees for ACA employer mandate purposes, and no FORM 1095-C is required. Self-employed status includes a sole proprietor, a partner in a partnership, and a 2-percent S corporation shareholder.
ELIGIBILITY & FULL-TIME STATUS
For TY23 ALEs are required to provide an affordable Offer of Coverage meeting both Minimum Essential Coverage [MEC] and Minimum Value [MV] to at least 95% of their Full-Time Employees. This means a value deemed comparable to insurance available on the open market and affordable [see below] based on their wages. ALEs therefore need to know which employees qualify as full-time.
» NOTE: Full-Time Equivalent [FTE] employee measures are not relevant here — only actual full-time employee status. Full-time equivalency is only used to determine an employer’s ALE status.
» IRS DEFINITIONS & METHODS:
A Full-Time Employee is one who works at least 30 hours of service a week or 130 hours a month. For this purpose, ‘hours’ include each hour an employee is paid or entitled to payment for performing duties for the employer or entitled to payment even if no work is done (such as paid vacation or sick time).
The IRS approves two methods for determining an employee full-time status. The Monthly Measurement Method and the Look Back Method.
» MONTHLY MEASUREMENT METHOD:
This is the preferred method for many employers, particularly with more structured workforces and a majority of Full-Time Employees. This method carries out month-by-month data processing of an employee’s hours to verify full-time status. Part-time employees in this method are also tracked on a monthly basis. When using this method, an offer of health insurance coverage must be made to workers within 90 days of the date they were hired.
The advantages of Monthly Measurement are efficiency and accuracy, reducing the end-of-year resource burden as well as enabling month-by-month error diagnostics and pro-active risk management.
» LOOK BACK METHOD:
This method works for employers with less clearly structured workforces and a shifting mix of part-time, full-time, and even seasonal employees. The Look Back Method is required to process eligibility for Variable Hour Employees [see above].
When using this method, a period of time known as the Measurement Period of between 3-12 months is chosen to ‘look back’ at each employee’s hours of service. Employees who average 130 hours per month during the Measurement Period are considered full-time and must be made an Offer of Coverage. This eligible status must be locked in during a subsequent period, which is known as the Stability Period (between 6 and 12 months but in no event longer than the Measurement Period).
TY23 AFFORDABILITY
As stated above, the employer’s Offer of Coverage to eligible employees must be affordable. The offer is deemed affordable if the employee’s required contribution for self-only coverage in the employer’s lowest cost plan does not exceed a specified percentage of the employee’s household income (even if the employee is enrolled in family coverage).
This affordability percentage was set at 9.12% for TY23.
Because employers do not know their employees’ household incomes, the ACA permits employers to determine affordability using certain Safe Harbor Methods as a proxy for household income.
CHOOSING AN AFFORDABILITY SAFE HARBOR
ALEs are not required to use the same Safe Harbor method for all Full-Time Employees. Different methods may be used for different business classifications as specified in the ACA regulations. But within each classification these Safe Harbor methods must be applied consistently; ALEs can’t apply different methods on an employee-by-employee basis.
Here is a quick guide to those different Safe Harbor methods:
- W-2: This Safe Harbor method generally maximizes the employee’s contribution. It works well: for a workforce whose earnings can be predicted with some certainty, and contributions can be structured as a percentage of weekly earnings. On the down side: this method can only be calculated after the close of the calendar year and is based on the employee’s income reported in W-2 BOX 1.
- RATE OF PAY: This method calculates affordability on a monthly basis, using the employee’s hourly rate of pay on the first day of the plan year. This method works well: for employer with significant number of hourly employees. On the down side: this method can’t be used for tipped and commission employees; and the Rate of Pay calculation is limited to 130 hours of service/montH.
- FEDERAL POVERTY LEVEL (FPL) : This is the simplest method but requires the highest employer contribution of the three Safe Harbors.
» TIP: Medical opt-out and wellness program incentives may impact affordability calculations and need to be properly structured to manage this impact.
NOTE ON RISK & AFFORDABLE COVERAGE: All an ALE’s potential penalty exposure for unaffordable coverage lies with eligible employees who waive coverage. The ACA penalty for unaffordable coverage is not automatic. The IRS 4980H[b] penalty is triggered only when an employee who has waived the unaffordable coverage on offer enroll in a Health Insurance Marketplace [also called Exchanges] to purchase coverage and benefit from a federal premium tax credit, lowering monthly payments. Employees enrolled even in unaffordable coverage [Form 1095-C Line 16,Code 2C] do not trigger the 4980H[b] penalty, because they would not be enrolled in a Health Insurance Marketplace with federal premium tax credit assistance.
So there you have it. The key CHANGES, TIPS & ERRORS for TY23 ACA compliance.
If you have questions about any aspect of the ACA process, please contact BENEFITSCAPE [the leading ACA specialist for employers on all major HCMs/ACA modules] at +1-508-655-3307 or info@benefitscape.com.
*Any sufficiently advanced technology is indistinguishable from magic. Arthur C Clarke
This guide was prepared with additional input by Richard A. Szczebak of RAS Law. It has been prepared as a general overview of the subject matter covered. It is not intended to provide, and should not be taken as, legal or compliance advice on any specific matter.



